An expert from the Danish Cancer Society, Kræftens Bekæmpelse, expresses doubt on the number of asbestos deaths in Denmark of 1300 annually, mentioned in the stories in the project Asbestos: The Lethal Legacy.

“I think the number of asbestos related cancer deaths nowadays in Denmark is lower, perhaps in the range of 300 annually,” says senior scientist, Ph. D. Johnni Hansen, Danish Cancer Society.
His main argument for this is that he finds the methods for calculation of the 1300 yearly asbestos related deaths to be outdated. Thus, the ban in Denmark on the use of asbestos developed gradually from 1972 to 1986. In the same period, the amount of asbestos, the number of exposed people and the exposure level decreased. Hence, it is over 50 years ago that asbestos exposure peaked in Denmark.
“It is scientifically well recognized that both lower exposure levels and cessation of exposure to lung carcinogens diminish the cancer risk. The same is not to the same extent valid for the rare cancer mesothelioma, which has been used as the main component for calculation of the 1300 current deaths per year,” stresses Johnni Hansen.
Therefore, he finds it unlikely, as calculated by “The Legal Legacy”, that over 1100-lung cancer deaths in 2019 are caused by asbestos exposure.
“In comparison, in total about 1900 men die each year from lung cancer in Denmark. Further, it is scientifically accepted that over 80% of lung cancers are caused by tobacco smoking,” Johnni Hansen emphasis.
Johnni Hansen points to a meta-study from 2019: “Risk of mesothelioma after cessation of asbestos exposure: a systematic review and meta-regression”, where the main conclusion was:
”This analysis provides evidence that the risk of mesothelioma does not decrease after cessation of asbestos exposure, while lung cancer risk does.”
He also points to a study from 2014: “The Risk of Lung Cancer After Cessation of Asbestos Exposure in Construction Workers Using Pleural Malignant Mesothelioma as a Marker of Exposure.“ This study concludes:
“Workers with heavy exposure to asbestos have a similar risk of lung cancer as persons with low or no exposure 20 years after the exposure has ended.”
Johnni Hansen finally points out he is pleased that there is a renewed focus on asbestos and the risk of cancer, including that the Danish Cancer Society historically and currently is working partly on epidemiological research, partly to focus on the prevention of asbestos-related cancer among construction workers in particular, and partly on compensation for those who get cancer from previous asbestos exposure.
The numbers of deaths in Denmark, of 1300 annually linked to exposure to asbestos, are part of a total estimate of all deaths in the world.
Several new studies show that the total number of deaths worldwide are around 250,000. In the project one of these studies was used, because it had the latest numbers.
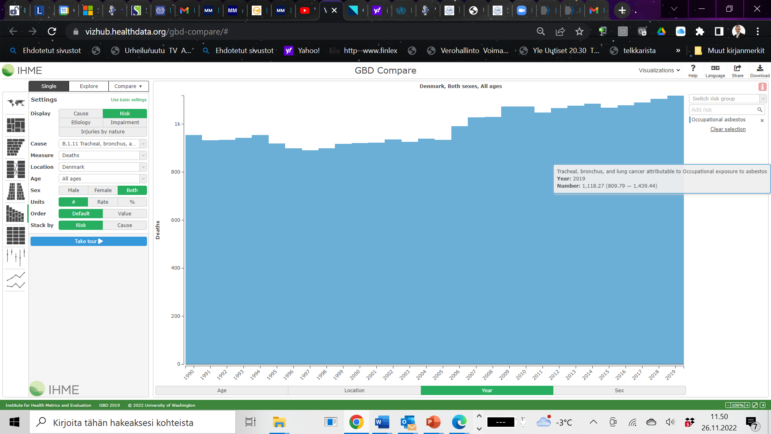
It was from the Institute of Health Metrics and Evaluation – Global Burden of Disease and Injury Programme at the University of Washington, GBD.

The investigation team worked together with Dr. Jukka Takala, who was one of around 1500 Global Collaborators, working with the Institute of Health Metrics and Evaluation.
Jukka Takala was previously the Director of the Global Programme on Safety and Health at Work at the International Labour Organisation (ILO). He is former president at the International Commission on Occupational Health, (ICOH), which numbers thousands of occupational health experts as members, as well as institutional members such as NIOSH, BAuA, INRS, HSE. Today he is the chair of the ICOH Occupational Cancer Working Group.
Many Danish collaborators are among that list of collaborators at GBD-program. The programme also works closely with the World Health Organisation (WHO) and national ministries and institutions.
“The founder and director of the programme is Dr Chris Murray, who originally worked at the WHO in establishing the data system there, and later moved to the USA to Seattle. The programme is strongly supported by Bill and Melinda Gates Foundation, while all the authors and collaborators are independent from such funding,” Jukka Takala tells Investigative Reporting Denmark.
The results of the cooperation have been published in the medical journal The Lancet, entitled GBD 2019 Risk Factors Collaborators*. Global burden of 87 risk factors in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet 2020; 396: 1223–49 (*For the list of Collaborators see Viewpoint Lancet 2020; 396: 1135–59). This is available online: https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(20)30752-2/fulltext and https://vizhub.healthdata.org/gbd-compare/ (accessed 29 November 2021).
Different latency period – long and permanent exposure
WHO/IARC Experts (McGregor, Peto, Byrnes, Straif, Boffetta) have also published a study on “Estimating the asbestos-related lung cancer burden from mesothelioma mortality“. Scientific estimates are using slightly different levels in establishing the asbestos exposure levels. The IHME estimate is 8.7 lung cancer deaths for one mesothelioma death. The calculation is much more complicated and different confidence intervals exist.
Jukka Takala agrees with Johnni Hansen that assessing death rates is difficult, because the mesothelioma latency period is much longer than that of lung cancer. “There are many opinions on the exact number of deaths. The European Parliament has a different view from the Commission and workers’ organisations do not agree with employers. I am confident with the GBD estimates. These may change with time but reflect today’s scientific opinion,” Jukka Takala explains.
“Science can be improved gradually and we will know better in 30-50 years but action is needed now for prevention. Renovations, demolishing, degrading of buildings and infrastructure takes place now and new and increasingly large populations are exposed,” he says.
“The average life expectancy is growing, which also expands the time in which people can develop diseases with long latency periods,” he adds.
Whilst no new asbestos can be used in the EU, since the ban came into force in 2005, existing structures that contain asbestos in densely populated areas, such as cities, may need to be either demolished or renovated, which is increasing the risk of exposure to damaged – and therefore dangerous – asbestos.
Furthermore, there is a continuously growing population that has been living and working in such buildings and infrastructure and also potentially inhaling fibres in the open air for 24 hours a day, for an increasing number of years.
“As asbestos exposure/lung cancer risk/outcome pair is based on a linear curve, a huge number of exposed workers/people will produce the same negative consequences now and in the future, similar to a small number of heavy exposures in the past,” Jukka Takala says.
He therefore suggest that the IHME numbers should be used by Danish authorities.

Another Danish expert, Chief Physician at Department of Occupational and Environmental Medicine at Aalborg University Hospital, Jakob Hjort Bønløkke says:
“I have a lot of faith in the expertise and calculations of Jukka Takala and his colleagues, but I also believe that there is a lot of truth in the argument from The Danish Cancer Society that lung cancer tends to develop faster and that the number therefore peaked earlier. This means that I personally do not think that the total number is quite as high as Jukka Takala and colleagues have calculated, but somewhere in between. On the other hand, there must have been many more additional lung cancer cases 20 years ago. But it is true, they have calculated it based on the scientific research in this field, so until some better research comes along, their data is the best we have.”
Lung cancer due to both smoking and asbestos
You probably wonder where the asbestos lung cancers are coming from when you don’t see them and – most likely – do not recognise and compensate those affected.
“The reasons are, apart from the exposure estimates based on mesothelioma numbers, as follows:
– Cancer is a disease, occupational cancer is an administrative decision
– Most asbestos deaths caused by lung cancer (not mesothelioma) are found among smokers; as a result a smoker having lung cancer cases are immediately suspected to be caused by smoking and the diagnosing doctors do not ask the Dr Ramazzini [the father of occupational disease] question: where did you work?” Jukka Takala points out.
Furthermore, only a tiny fraction of lung cancer victims undergo a thorough postmortem examination; even less of the lung asbestos fibre tissue samples are counted from the lungs of the deceased if asbestos exposure is not suspected.
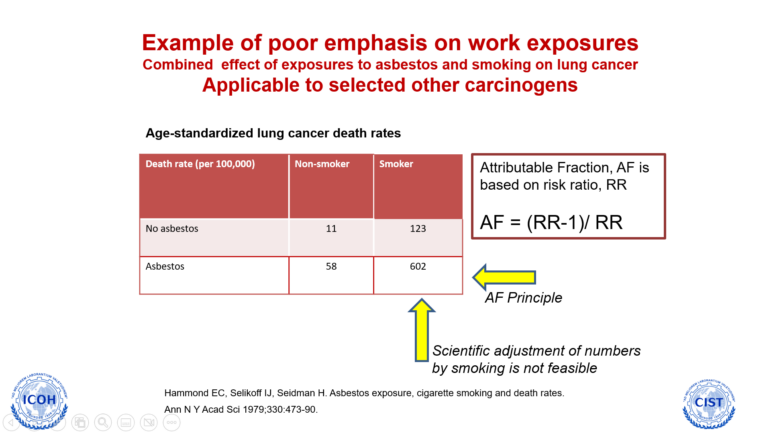
“This means also that a huge majority of deaths can be avoided by eliminating asbestos exposure and an even larger number in eliminating smoking. Asbestos exposure, however, is an occupational risk, whereas smoking is an individual decision,” Jukka Takala says.
In many developed countries a common practice is that one cannot discriminate smokers when considering compensation but in practice the asbestos related cases are not identified and diagnosed and not known by the victims themselves or their relatives.
More background on the method
Below find some related links to the IHME/GBD projects:
“Estimation of the global burden of mesothelioma deaths from incomplete national mortality data”